Diabetes Type 2: Symptoms, Causes & Treatment Options
What Is Diabetes Type 2?
Type 2 diabetics have a hard difficulty converting glucose (sugar) from food into energy. Type 2 diabetes is a chronic illness that prevents your body from properly utilizing insulin. Insulin resistance is a term used to describe people who have type 2 diabetes.
This type of diabetes is most common in middle-aged and older people. It was previously known as adult-onset diabetes. However, type 2 diabetes affects children and teenagers, owing to childhood obesity.
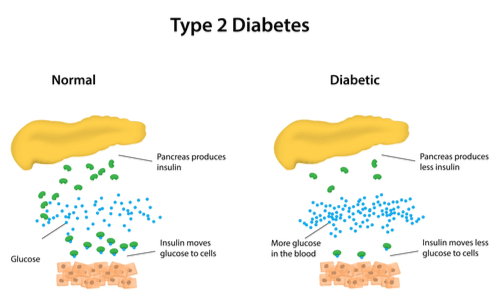
Carbohydrates in meals are broken down into glucose after we consume them. Blood sugar levels rise when glucose enters the bloodstream. The pancreas then releases insulin into the bloodstream. Insulin aids in the opening of cells throughout the body, allowing glucose to enter and provide energy to the cells.
The pancreas produces insulin, but the cells do not respond to it as they should in type 2 diabetes. Insulin resistance is the term for this. Blood sugar levels rise when glucose cannot enter cells. The pancreas then works even harder to produce even more insulin. The additional insulin initially preserves sugar levels in the normal range. However, the pancreas can no longer keep up, and blood sugar levels remain high. Type 2 diabetes develops when blood sugar levels remain high.
Type 2 Diabetes Signs and Symptoms
Type 2 diabetes symptoms might be so subtle that they go unnoticed. Approximately 8 million people are unaware that they have it. Among the signs and symptoms are:
- Being extremely thirsty
- Frequently peeing
- Vision is hazy
- Being irritable
- Numbness or tingling in your hands or feet
- Feeling tired/fatigued
- Wounds that refuse to heal
- Yeast infections that do not go away
- Feeling hungry
- Weight loss without exerting effort
- Developing new infections
Consult your doctor if you experience dark rashes around your neck or armpits. These are known as acanthosis nigricans and can indicate that your body is becoming insulin resistant.
Type 2 Diabetes Causes
Insulin is a hormone produced by your pancreas. It aids your cells in converting glucose (a type of sugar) from your food into energy. Type 2 diabetes patients produce insulin, but their cells do not use it as efficiently as they should.
To get glucose into your cells, your pancreas produces more insulin initially. But it cannot keep up forever, and glucose builds up in your bloodstream.
Type 2 diabetes is usually caused by a combination of factors. Some examples are:
- Genes. Different pieces of DNA (Deoxyribonucleic acid) that control how your body generates insulin have been discovered by scientists.
- Extra pounds. Insulin resistance can be caused by being overweight or obese, especially if you carry additional pounds around your belly.
- Syndrome metabolic. Insulin resistance is associated with a slew of symptoms, including high blood sugar, belly fat, high blood pressure, and high cholesterol and triglycerides.
- Your liver is producing too much glucose. When your blood sugar falls below a certain level, your liver produces and releases glucose. Your blood sugar rises after you eat, and your liver slows down and stores the glucose for later. Some people’s livers, however, do not. They continue to produce sugar.
- Cellular communication is poor. Cells can send incorrect signals or do not receive messages correctly. A chain reaction can result in diabetes if these issues alter how your cells create and utilize insulin or glucose.
- Beta cells that are broken. Your blood sugar is thrown off if the cells that generate insulin send out the wrong quantity of insulin at the wrong time. High blood sugar levels can also harm these cells.
What Causes Type 2 Diabetes in Some People?
Nobody knows why some people get type 2 diabetes, but it is a combination of genetics and environmental factors. Many children who contract it have a family member who also has it.
Children are more likely to develop type 2 diabetes:
For those who are obese Sugar in the blood does not get into the cells as well as it should when a person is overweight. Type 2 diabetes can strike anyone, regardless of weight.
During adolescence Around puberty, many children and teenagers are diagnosed with type 2 diabetes. Insulin resistance develops as growth hormone levels rise during adolescence.
Polycystic ovarian syndrome (PCOS). Girls and women with PCOS are more likely to develop type 2 diabetes than those whose moms had diabetes during pregnancy. When a mother develops diabetes, her babies are exposed to extra sugar in the womb. This, in combination with genetic factors, raises the risk of developing type 2 diabetes later in life.
Risk Factors for Type 2 Diabetes
Certain factors increase your chances of developing type 2 diabetes. The more of them that apply to you, the more likely you are to receive them. Some items are linked to your identity:
- 45 years old or older
- Family, a diabetic parent, sister, or brother
Other factors that increase your diabetes risk include your daily behaviors and lifestyle. These are the ones over which you have control:
- Little or no physical activity
- Smoking
- Stress
- Too little or too much sleep
- Ethnicity. Asian American, African American, Alaska Native, Native American, Hispanic, or Latino, or Pacific Islander American
The following are health and medical history-related risk factors:
- Prediabetes
- Diseases of the heart and blood vessels
- Even if it is treated and under control, high blood pressure can be dangerous.
- HDL (“good”) cholesterol levels are low.
- Triglycerides high
- Obesity or being overweight
- Having a child who was more than 9 pounds
- Having gestational diabetes when pregnant
- Ovarian polycystic syndrome (PCOS)
- Depression
What is the Treatment for Type 2 Diabetes?
Children and teenagers with type 2 diabetes frequently seek therapy from a pediatric endocrinologist. This type of specialist specializes in hormone-related issues such as diabetes. A nutritionist, diabetes educator, or weight management specialist may also be consulted.
The goal of type 2 diabetes treatment is to keep blood sugar levels within a healthy range. Typical treatment includes:
- consuming a well-balanced diet
- doing regular exercise checking blood sugar levels on a regular basis decreasing weight, and if necessary, taking anti-diabetes medicines or insulin (by injection or with a pump). If blood sugar levels continue to rise, the doctor may prescribe another medication.
What Problems Can Type 2 Diabetes Cause?
Sugar levels that are too high or too low might cause:
- hyperglycemia. When blood sugar levels are excessively high, this occurs. Hyperglycemia can make children thirsty and cause them to pee more than usual. If high blood sugars are not addressed, children can get ill and develop health problems later in life, such as heart and kidney disease.
- Ketoacidosis in diabetics (DKA (diabetic ketoacidosis)). This dangerous ailment requires immediate attention. When the body lacks enough insulin to allow glucose into the cells, the body begins to break down fat rather than sugar. Nausea, vomiting, stomach pain, rapid breathing, and, in extreme situations, unconsciousness are also symptoms of DKA.
- DKA affects persons with type 1 diabetes more frequently, however, it can also affect children with type 2 diabetes.
- hyperosmolar hyperglycemic condition (HHS). This is a dangerous disorder that, like DKA, requires immediate treatment. HHS patients have acute dehydration and extremely high blood sugar levels.
- hypoglycemia. When blood sugar levels are too low, this occurs. When persons with type 2 diabetes are treated with insulin, this can happen. If a diabetic receives more insulin than they require, their blood sugar level may go dangerously low. Headaches, weakness, shakiness, anxiousness, and sweating are some of the symptoms.
What Can Parents Do to Help?
It may take some time for your child and family to become used to having type 2 diabetes. Your child and you will learn everything you need to know about staying healthy from the care team. Taking your child to all their doctor’s appointments and sticking to the diabetes treatment plan will help you stay on track.
It can feel overwhelming when your child gets type 2 diabetes, but you are not alone. You and your child will be looked after by the diabetes care team. Contact them if you have any queries or need assistance.
Medication
If lifestyle changes are not enough to get you to your goal blood sugar levels, medication may be required. The following are some of the most prevalent symptoms of type 2 diabetes:
- Metformin is a drug that is used to treat diabetes (Fortamet, Glucophage, Glumetza, Riomet). This is typically the first treatment for type 2 diabetes. It helps your body respond better to the insulin it does make by lowering the quantity of glucose your liver produces.
- Sulfonylureas. This class of medications aids in the production of insulin in the body. Glimepiride (Amaryl), glipizide (Glucotrol, Metaglip), and glyburide are some of them (DiaBeta, Micronase).
- Meglitinides. They aid in the production of insulin and are more effective than sulfonylureas. Nateglinide (Starlix) or repaglinide are two options (Prandin).
- Thiazolidinediones. They, like metformin, increase insulin sensitivity.
- Pioglitazone (Actos) or rosiglitazone (Rosiglitazone) are two options (Avandia). However, because they increase your risk of cardiac problems, they are not normally the initial therapeutic option.
- Inhibitors of DPP-4. These drugs — linagliptin (Tradjenta), saxagliptin (Onglyza), and sitagliptin (Januvia) — reduce blood sugar levels but can potentially cause joint discomfort and pancreas inflammation.
Agonists for GLP-1 receptors. These drugs are administered through a needle to slow digestion and lower blood sugar levels. Exenatide (Byetta, Bydureon), liraglutide (Victoza), and semaglutide are three of the most frequent (Ozempic).
Inhibitors of SGLT2. These aid in the removal of more glucose from your kidneys. You could be prescribed canagliflozin (Invokana), dapagliflozin (Farxiga), or empagliflozin (Empagliflozin) (Jardiance). Empagliflozin has also been shown to reduce the risk of heart failure-related hospitalization or mortality.
