Diabetic Neuropathy: The Silent Enemy Of Diabetes Patients

Getting diabetes complications is scary. But following your treatment plan, asking for help when you need it, and doing other things like getting tested for high blood pressure will help keep that from happening.
People with diabetes can develop diabetic neuropathy. This is when nerves in your feet and hands are damaged. Diabetic neuropathy symptoms include numb sensations, pain, and tingling especially at night or in the morning. You can get it in one area or all over. The damage can affect any part of your body including the digestive system, urinary tract, and blood vessels as well as your heart.
Diabetic neuropathy is a serious complication of diabetes that can occur around the nerves in your legs and feet. As many as 50% of people with diabetes may develop it but you can often prevent diabetic neuropathy or slow its progress by keeping your blood sugar levels under control, exercising regularly, and getting checkups at least once a year.
Type of Diabetic Neuropathy and their Symptoms
Neuropathy is the most common complication of diabetes. Symptoms may include problems with sensation, movement, and feeling.
There are four main types of diabetic neuropathy:
- Diabetic Autonomic Neuropathy (also called Sympathetic or Retroperitoneal Neuropathy)
- Peripheral Neuropathy (or Peripheral Nervous System Neuropathy)
- Proximal Neuropathy (or Upper Motor Neuron Disease)
- Cranial Neuropathy.
Autonomic neuropathy
If you have signs and symptoms of autonomic neuropathy, your diabetes may not be well controlled. You can help prevent nerve damage by making sure to keep your blood glucose levels within the recommended range as much as possible.”
Hypoglycemia (low blood sugar) is a common problem for people with diabetes. Hypoglycemia can be uncomfortable, even painful if it is not recognized and treated. The symptoms often start before your blood sugar reaches a dangerously low level. Some symptoms may indicate an oncoming episode of hypoglycemia.
You may notice changes in your vision, such as blurriness, double vision, or trouble adjusting from light to dark or far to near. These symptoms may be due to a drop in blood pressure caused by the medications you are taking. This is a common side effect and should pass after a few days.
Peripheral neuropathy
Peripheral neuropathy may be the most common diabetic complication. It is a condition that damages the nerves in your feet, legs, hands, and arms. Signs and symptoms of peripheral neuropathy include pain from nerve damage, numbness or tingling in the limbs, muscle weakness, loss of balance and coordination, abnormal skin sensations such as burning or itching, and changes in your ability to feel hot or cold
Signs and symptoms of peripheral neuropathy include numbness, tingling, and pain that can be felt on the shoulders and hips. The most common sign is a pain in your feet upon waking that gets better throughout the day. Other symptoms may include changes in your ability to feel heat or cold, sharp pains or cramps, muscle weakness, and extreme sensitivity to touch even light contact like bed sheets could cause pain.
Mononeuropathy (focal neuropathy)
Mononeuropathy means damage to a single nerve. It is a form of focal neuropathy. Mononeuropathy may lead to numbness, tingling, and/or weakness in the face, hand, or foot. This can cause difficulty walking or standing up straight. You may also notice pain in your ankle or heel (shin splints) if you overuse it. Mononeuropathy may also result in muscle wasting (atrophy).
Proximal neuropathy (diabetic polyradiculopathy)
Diabetic polyradiculopathy is the most common form of diabetic neuropathy and can cause severe pain in the buttock, hip, or thigh. It can also affect the abdominal and chest area. The pain is often on one side of the body but may spread to the other side. Symptoms are usually caused by damage to the nerve that carries messages from your spinal cord to nerves in your legs and feet. This type of damage may cause you to have difficulty rising from a sitting position, and have weakened thigh muscles and chest or abdominal wall pain.
When is the right time to see a doctor?
If you have foot pain: Take a break from activities that hurt your foot. If the pain is severe, call your health care provider so he or she can give you advice on treatments. If the pain is mild, you may be able to treat it with simple home remedies like rest, ice, compression, and elevation. You also may want to use no steroidal anti-inflammatory medications for pain relief.
The American Diabetes Association recommends that screening for diabetic neuropathy begin immediately after someone is diagnosed with type 2 diabetes or five years after diagnosis with type 1diabetes. The ADA also recommends that you get a screening once a year after that.
Causes of Diabetic Neuropathy
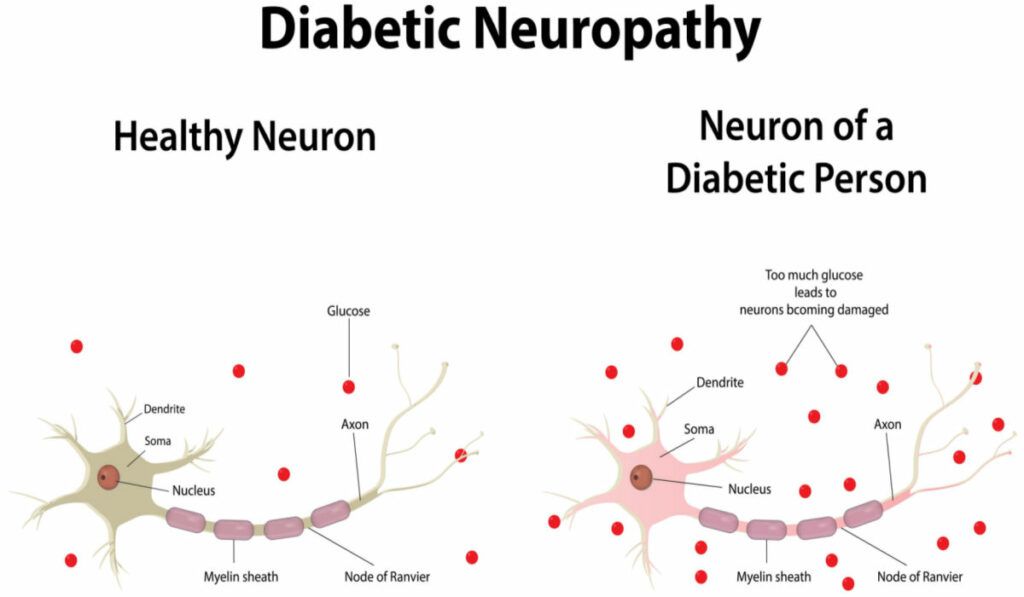
The causes of diabetic neuropathy are not completely understood. Researchers think that diabetes causes high blood sugar to flow through your body. Over time, high blood sugar damages nerves and interferes with their ability to send signals, leading to nerve damage or diabetic neuropathy. High blood sugar also weakens the walls of the small blood vessels that supply nerves with oxygen and nutrients.
Risk factors of Diabetic Neuropathy
Diabetic neuropathy, which affects the nerves that control sensations in your hands and feet, can cause numbness and tingling. Diabetes can also damage the blood vessels in the brain, causing stroke and other serious problems.
Although the causes of diabetic neuropathy are not clear, some underlying factors can increase the risk of developing this condition including kidney disease, diabetes, being overweight, smoking, and nerve damage from previous injury or surgery. The good news is that there are ways to prevent or postpone the symptoms of diabetic neuropathy. Make sure to check with your doctor before taking any of these steps.
What are the Serious Complications?
Diabetic neuropathy can cause a few serious complications, including:
- Diabetic neuropathy can cause a number of serious complications. Some of these complications such as hypoglycemia unawareness are dangerous because they may require urgent medical attention to prevent more severe problems such as unconsciousness or death.
- You should always alert your doctor of any swelling, redness, or discharge from your injury. Nerve damage that cannot be treated will lead to a loss of feeling in your feet, so even minor cuts could turn into sores or ulcers without being noticed. In severe cases, the infection can spread to the bone or lead to tissue death requiring amputation.
- Urinary tract infections are common, and often go undiagnosed because they may have no symptoms. Left untreated, however, they can cause serious kidney damage and may lead to complications like sepsis (blood poisoning). Urinary incontinence is often caused by a weak bladder muscle that may be due to nerve issues. The nerves issues can also give you trouble controlling your muscles that release urine.
- People with chronic hypertension have a fourfold increased risk of stroke, the third-leading cause of death in the world. A significant drop in blood pressure when standing after sitting or lying down is a condition called orthostatic hypotension. It can lead to lightheadedness and fainting, which can result in injuries such as falls and fractures.
- A slow stomach emptying leads to bloating, indigestion, and discomfort. The nerves in the digestive tract control how quickly food passes through this area of your body. Diabetes-related nerve damage can lead to gastroparesis which is a condition in which the stomach empties too slowly or not at all. This can cause bloating and indigestion.
- Sexuality can be affected, and this can cause problems in relationships. If you have autonomic neuropathy and are having sexual difficulties, it is important to talk with the healthcare professionals involved in your care and with your partner.
- Increased or decreased sweating can result from a number of different factors. Nerve damage can disrupt how the sweat glands work and make it difficult for the body to control its temperature properly. Damage to other parts of the body, such as joints or muscles, can also affect how much you sweat because your body needs this moisture to stay cool.
How to Prevent?
Although it is not an inevitable result of diabetes, diabetic neuropathy – is a common complication that results in foot pain and can lead to amputation. The good news is that you can prevent or delay the development of diabetic neuropathy by closely managing your blood sugar and taking good care of your feet.
Blood sugar management
The glycated hemoglobin (A1C) test reflects your average blood sugar level over the past 2 to 3 months. The American Diabetes Association (ADA) recommends that people living with diabetes have an A1C test at least twice a year. Checking your blood sugar levels can help you protect your health and prevent complications from uncontrolled diabetes
Foot care
As a person with diabetes, it is important to take care of your feet. Problems like sores that will not heal, ulcers, and even amputation can become more common if you have diabetic neuropathy. To prevent these problems, have a thorough exam at least once a year and see your health care provider when symptoms begin to appear. Healthy feet are important to your overall health. Your health care provider may recommend foot care products that you can use at home to help keep your feet clean and dry.
